Inaccessibility to health care key factor in COVID-19's devastating toll on Indigenous communities
‘So much loss’
Carol Schumacher of the Navajo Nation had grappled with untimely deaths; her mother died at 65 of pulmonary disease, and her father died at the same age in a car crash caused by a drunken driver. But she was not prepared for the devastation of Covid: Since it arrived in the U.S. more than two years ago, she has lost 42 family members to the virus.
Dealing with the massive death toll strained her own health, Schumacher told our colleagues. “I just wasn’t mentally prepared to deal with so much loss,” she said.
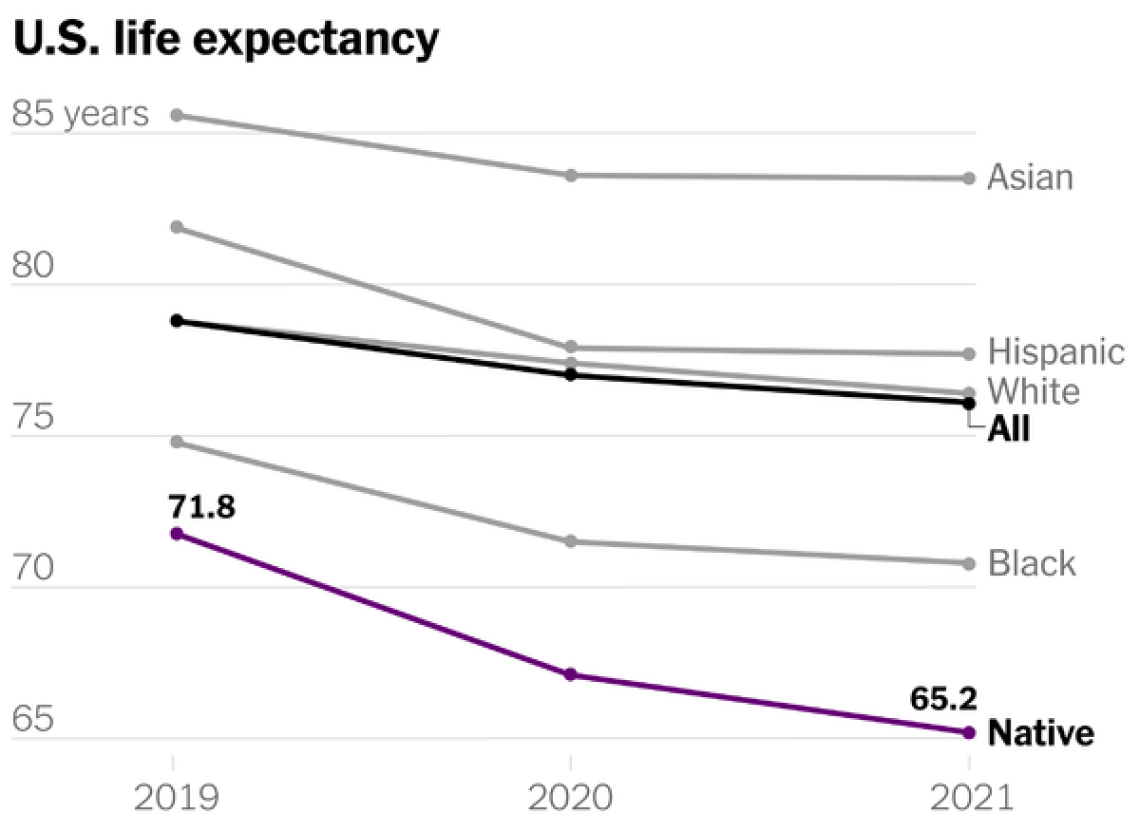
That loss has been tragically common among Native Americans, the C.D.C. revealed last week: From 2019 to 2021, their life expectancy fell from 71.8 years to 65.2. Covid was largely to blame.
Typically, experts start to worry when they see drops in life expectancy that measure in just tenths of a year; Native Americans lost nearly seven years. The drop erases the equivalent of more than four decades of American life expectancy gains. And the average Native American person is now expected to live as long as the average American did in 1944.
There is no one explanation for Covid’s death toll in these communities. But the main causes appear to involve poverty. Native Americans tend to have higher rates of underlying health problems that exacerbate Covid, as well as worse access to health care.
“Even prior to the pandemic, rates of death among Indigenous people were higher in lots of categories,” said Dr. Laura Hammitt, an epidemiologist at Johns Hopkins University. Covid magnified those health disparities, causing a drop in life expectancy with no modern precedent in the U.S.
Historical problems
Since vaccines became available, Covid deaths among Americans have typically tracked closely with vaccination rates. For example, resistance against vaccines in predominantly Republican communities has led to more Covid deaths in recent months among white Americans than among Black or Hispanic Americans — a shift from the early days of the pandemic, as this newsletter has explained.
The link breaks down when it comes to Native Americans. Vaccination rates among Native Americans are higher than they are among Black or Hispanic Americans, according to C.D.C. data. Yet Native Americans have died from Covid at one of the highest rates of any race or ethnicity since the start of the pandemic:
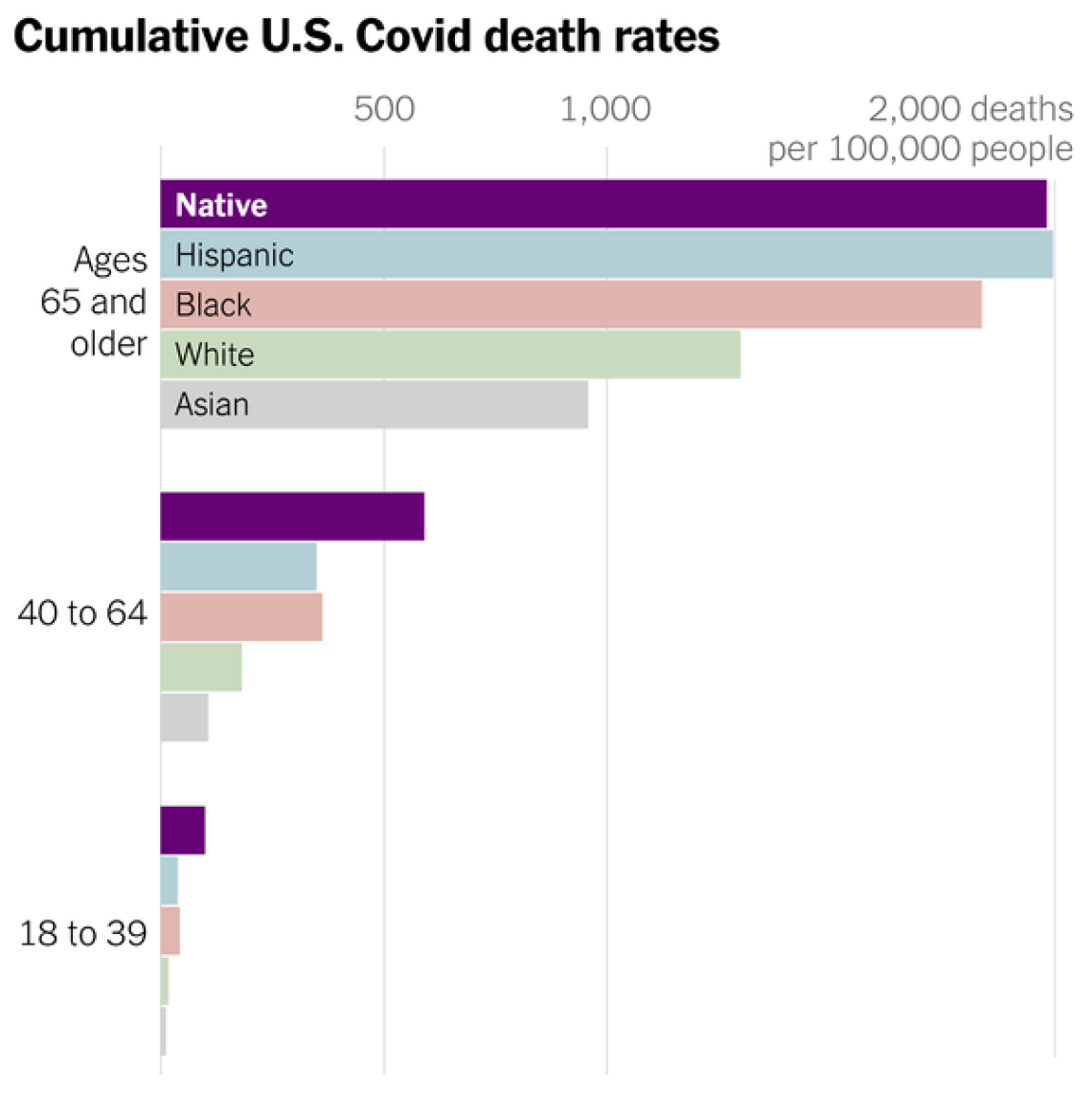
Experts say other factors, besides vaccination rates, are to blame.
Among them: Native Americans have some of the highest rates of health conditions, such as obesity and diabetes, that make a person much more likely to die from Covid.
Health care is also often inaccessible. The Indian Health Service, a federal program that provides care to more than two million Native Americans, has a fraction of the funding on a per-person basis received by Medicare, Medicaid or the Veterans Health Administration. “How can somebody think this is not a problem? Yet it’s become normal,” said Loretta Christensen, the service’s chief medical officer.
As a result, Native Americans frequently have to travel long distances to get health care. Its quality can be shoddy. A quarter of Native Americans reported experiencing discrimination when visiting a doctor or a health clinic, one poll found. Cultural and language barriers can also make it difficult for Indigenous people to get the care they want. Given those obstacles, some try to tough out illness at home, with potentially deadly results.
Poverty can play a more direct role, too. Roughly one in four Native Americans live in poverty. The stress from it can worsen health, studies have found.
Consider Arizona, one of the states with the highest share of Native Americans. There, the highest Covid death rates strongly overlap with counties where more Native Americans live and where poverty is the highest. They also correlate with the places with the least access to internet (a sign of economic neglect):
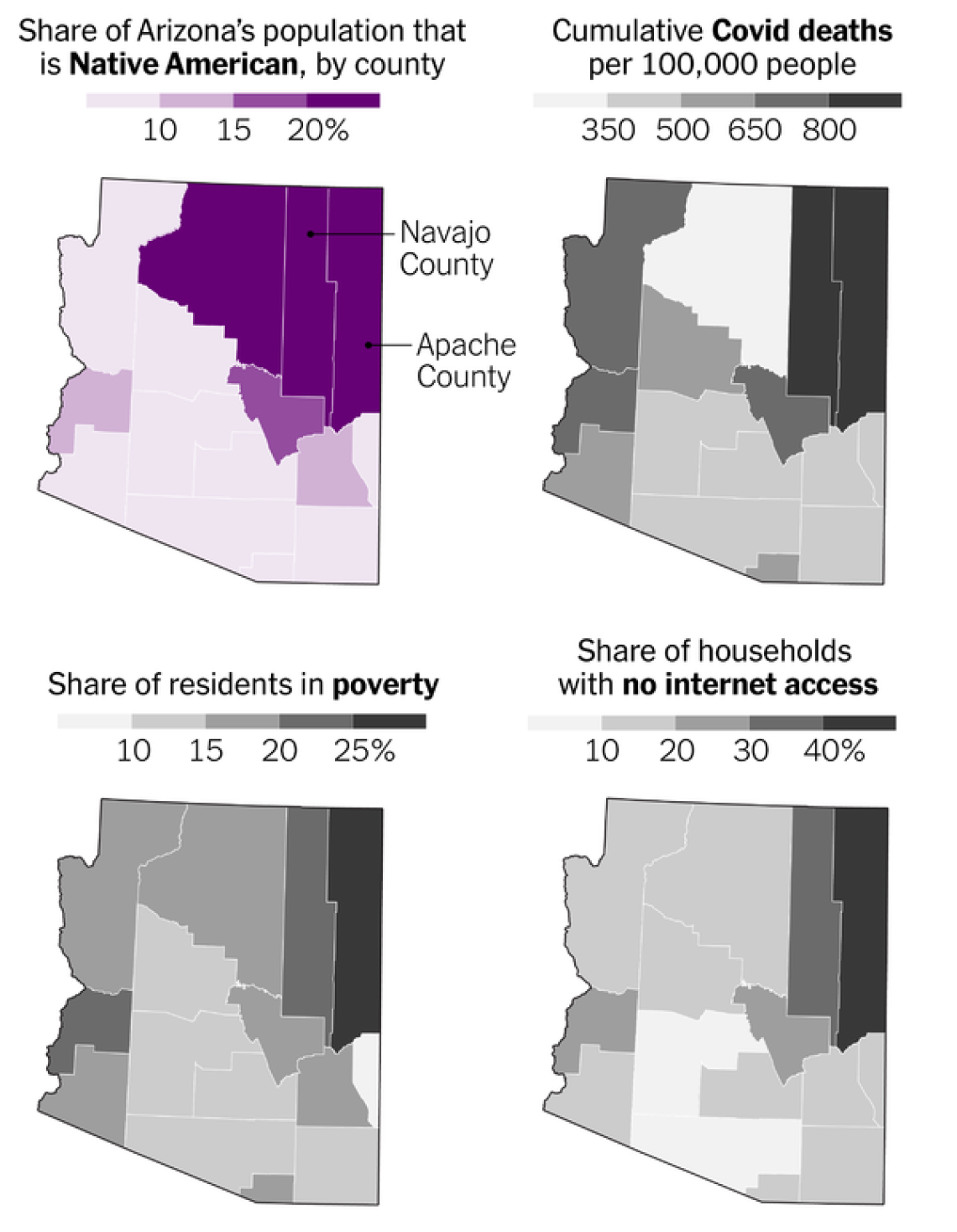
Widespread poverty limits what precautions people can take to avoid Covid. People living paycheck to paycheck can’t afford to take time off work to avoid spreading or catching the virus. Native Americans also often lack access to internet, electricity and running water — making remote work, virtual schooling or telemedicine impossible.
And Native Americans often live in crowded, multigenerational homes. So if they are sick, they can easily spread the virus to the rest of the family, including older relatives who are much more vulnerable to Covid.
In other communities, the presence of one or some of these issues has made Covid deadlier. But Native Americans are dealing with all of these problems at once — the kinds of conditions that allow a pandemic to flourish.
The suffering of Native Americans shows that preventing deadly pandemics isn’t just about containing the pathogens that cause them, but also about improving the health of communities across the board.
For now, the vaccines offer the best protection against severe illness from Covid. Now that the federal government has authorized the next generation of Covid vaccines, the most important step people can take to protect themselves is to get their shots.

