Are you covered by Medicaid? Here's what to know about possible coming cuts
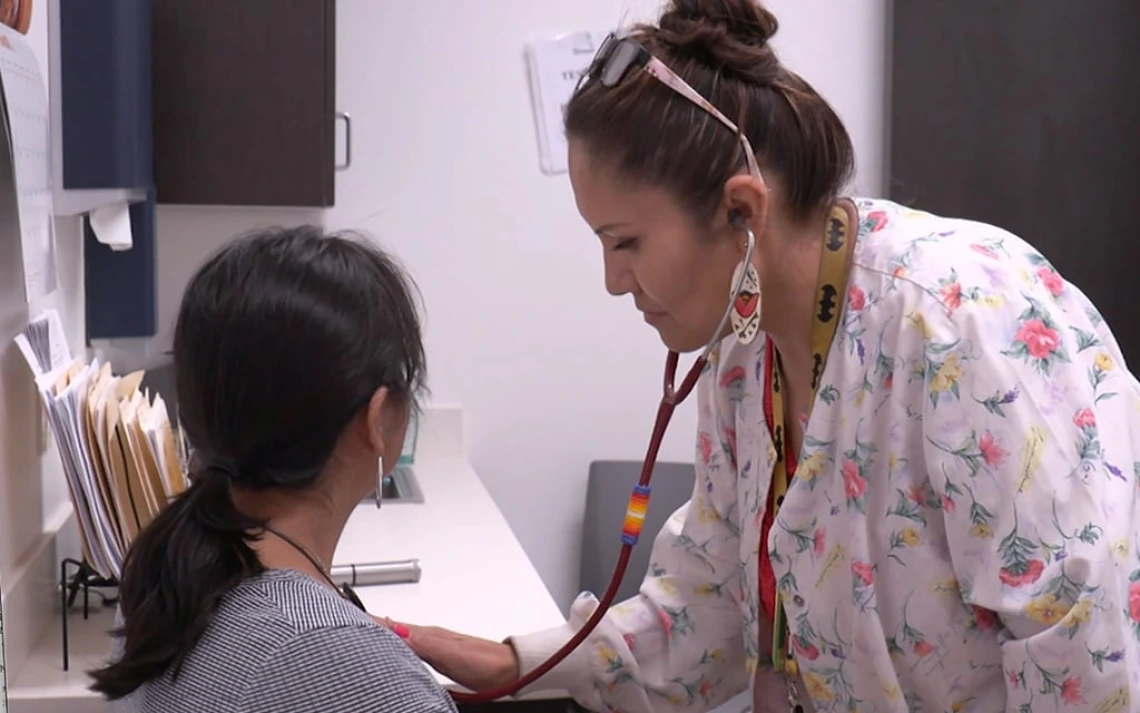
Dr. Derksen Quoted
More than half a million Arizonans could lose their health coverage if President-elect Donald Trump and a Republican-controlled Congress target Medicaid expansion when they look for ways to cut federal spending.
Changes to Medicaid are expected under a second Trump administration and a potential target for spending cuts is the Medicaid expansion that was allowed through the federal Affordable Care Act, according to a Nov. 27 analysis by KFF, an independent health policy research and information organization.
Arizona is one of nine states with a so-called "trigger law" that would automatically repeal its Medicaid expansion program if enhanced federal funding drops to various levels below 90%, research by the KFF and the Georgetown Center for Children and Families says.
In Arizona, the trigger for the Medicaid expansion population activates when federal matching funds dip below 80%, which would be a significant blow to the Arizona program and could remove coverage for thousands of enrollees.
Medicaid is health insurance for primarily low-income people and in Arizona, it is a $21 billion program that enrolls 2.1 million people and is known as the Arizona Health Care Cost Containment System, or AHCCCS (pronounced "access").
About 71% of the program's funding comes from the federal government and the remainder comes from various sources, including the state general fund, tobacco tax money and counties.
Medicaid expansion allowed more people to qualify for the government-funded program by expanding the qualifications to those earning up to 138% of the federal poverty level, or $20,783 per year for an individual.
The adult Medicaid expansion population in Arizona is 70,866 people. An additional population of 448,592 childless adults is likely to be affected by a drop in enhanced federal funding because of a hospital assessment that the federal funding drop would eliminate.
Critics say repealing Medicaid expansion is among the possible actions on health care under Trump that would return hospitals to an era when emergency departments were filled with very sick, uninsured patients and when hospitals' budgets were stretched by providing uncompensated care.
Other potentially affected states with trigger laws are Arkansas, Illinois, Indiana, Montana, New Hampshire, North Carolina, Utah, and Virginia, KFF reporter Phil Galewitz wrote Dec. 4.
Arizona Gov. Katie Hobbs is aware of various proposals "threatening jobs and access to health care for everyday Arizonans," a spokesperson wrote in an email.
"While we won’t engage in hypotheticals, the Governor’s Office is working with stakeholders to ensure they are aware of the ramifications of the various proposals and the devastating impact they could have on Arizona families and our economy," Christian Slater wrote.
When people can't get health insurance, hospitals and providers pay
If 70,866 or more Arizonans lose AHCCCS coverage and can't afford to purchase their own health insurance, the result would be what's known as "cost shifting," where health care expenses shift from the government program to the hospital and provider system that will have to give uncompensated care to uninsured people, said Dr. Daniel Derksen, a health policy expert who is director of the Arizona Center for Rural Health at the University of Arizona.
"If you price people out of the market, guess what happens. They go without and when they do get sick, you are talking about the hospitals, the physicians and others shouldering a higher burden of charity care and uncompensated care," Derksen said. "So you are not really saving money. You are just shifting who has to pay for the cost of that care to the providers and the hospitals."
When Arizona passed Medicaid expansion in 2013 under then-Republican Gov. Jan Brewer, it not only increased the AHCCCS income limit but also restored coverage for childless adults who had lost their coverage during state budget cuts in 2011, which resulted in hundreds of thousands more Arizonans gaining coverage.
A potential drop in enhanced federal funding for Medicaid expansion would also repeal the Arizona Hospital Assessment, which is the primary source of funding for the childless adult population, AHCCCS officials say. The childless adults on Medicaid, who number 448,592, are often known as the Proposition 204 population, in reference to a 2000 voter mandate that the state provides health care for everyone below the federal poverty level.
Medicaid is not the only health care program that could be on the chopping block when Congress reconvenes and a new presidential administration assumes control of federal agencies. Federal subsidies that have significantly reduced monthly premiums for health insurance marketplace plans offered through the Affordable Care Act, known as the ACA, are set to expire at the end of 2025. ACA health plans are also sometimes called Obamacare.
Without enhanced ACA subsidies and with Medicaid cuts, Derksen said, Arizona's rate of uninsured people would likely end up "pretty close to where we were before the Affordable Care Act. I think we'd be at between 18% and 20% uninsured, potentially one in five Arizonans being uninsured (versus an uninsured rate of between 9% and 11% now)," he said "That's the kind of math that closes our rural and critical access hospitals."
This article was originally published by the Arizona Republic

