Phoenix Children’s Hospital no longer in-network with major insurance provider
With no renewal agreement, that means the end of in-network insurance coverage for those patients insured by AZ Blue.

PHOENIX — The health insurance contract between BlueCross BlueShield of Arizona and Phoenix Children’s Hospital has expired.
Without a renewal agreement, in-network insurance coverage for patients insured by AZ Blue will end.
12 News got a statement from AZ Blue saying, “With Phoenix Children’s deciding to leave the network effective October 31, 2024, our priority is our members and their children who need care.”
According to AZ Blue’s Chief Medical Officer, Dr. Cara Christ, this comes after no agreement was reached regarding a 50 million dollar raise that would be a 10% increase for the next three years, which AZ Blue wanted.
“BlueCross BlueShield is no longer an in-network provider with Phoenix Children’s and we’ve prepared this page on our website to encourage patient families to seek continuity of care and review what plans are in our network,” Phoenix Children's told 12News Thursday.
These locations will become out-of-network starting Oct. 31 meaning it will cost more for AZ Blue patients:
- Phoenix Children’s Hospital Thomas campus
- Phoenix Children’s Hospital Arrowhead campus
- Phoenix Children’s Medical Group
- Phoenix Children’s Pediatrics
- Phoenix Children’s Urgent Care centers.
“We know we’re getting the best care around here and for them to not come to an agreement is a slap in the face,” Shelle Harman of Glendale said. “They obviously do not actually care about our family.”
Glendale’s Shelle Harman has a 10-year-old son Braxton who has a larger-than-life personality despite having a cyst on his brain and all down his spine and an autoimmune disorder. Braxton has 16 different doctors through Phoenix Children’s along with scheduled IVIG operations every 3-4 weeks to help him live what he’s been doing for the past six years.
"There’s no other hospital in the area that we would be able to find all those 16 doctors,” Shelle added. “We will have to try to find a new immunologist. And for those kind of specialty doctors, you’re not going to be able to get in for six months to a year.”
Now Shelle is considering going to other states for care because no agreement was made and it’s cheaper than paying out-of-network costs.
“Braxton and I would have to travel out of state to go to whatever doctors we can find,” Shelle said. “I think California and Texas Children’s is really good or Boston or Seattle would be our options for that kind of care. Cardon Children’s Medical Center and Banner Children’s doesn’t even rank for a children’s hospital.”
Care will continue for AZ Blue patients currently in treatment or with already approved and scheduled surgeries at Phoenix Children’s. Additionally, the emergency room will still be covered as in-network.
For more information, you can click here to visit Phoenix Children's website.
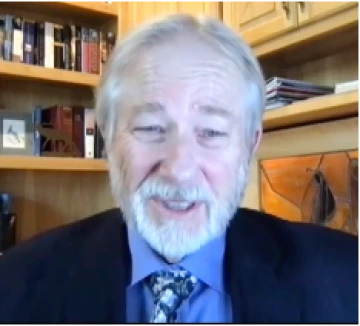
Dr. Daniel Derksen, the director of the University of Arizona’s Arizona Center for Rural Health, said he believes an agreement will eventually be reached. It took PCH and insurance company Aetna two months to reach a deal after their agreement lapsed in 2023.
“What’s needed is accountability and better data on what is a reasonable benefit package, what’s a reasonable rate, what’s reasonable charges versus payment rates, and I’d like to see more transparency,” Derksen said. “You know, a lot of us will drive extra miles just to get five cents a gallon cheaper on our gas, and there’s not that transparency and accountability in healthcare,” Derksen said.
Phoenix Children's issued the following statement:
“Phoenix Children’s contract with BlueCross BlueShield expired on October 30, 2024, and a new agreement is unlikely. Yes, we turned down BlueCross BlueShield’s offer, and here’s why. BlueCross BlueShield’s fictional offer of $80 million is closer to $43 million when we account for several factors including wrongful denials. BlueCross BlueShield denies more than 10% of claims submitted by Phoenix Children’s, resulting in annual reductions of $21 million and growing.
This includes frequent arbitrary denials of medically necessary services, causing undue stress, worry, and delays for the families we serve. Despite our multiple requests, BlueCross BlueShield is unwilling to have a qualified, independent pediatric physician review the claims before denying services or payment. We cannot allow this to continue.
We also said no to BlueCross BlueShield’s scheme to move families to restrictive, narrow networks and their exclusion of Phoenix Children’s from the state-wide PPO network. Such network limitations would have a devastating impact on families and force them into restricted coverage and access to quality services.
In addition to restricting access to its members, BlueCross BlueShield wants to make unilateral changes to the contract terms and rates after the contract has been agreed to and signed. We cannot allow BlueCross BlueShield to unilaterally amend and implement new contract terms and rates without the mutual written consent of both parties.
Instead of negotiating in good faith, BlueCross BlueShield left the contract discussions early and is spending time disseminating false information to alarm patient families and avoid discussing contract language that fundamentally impacts the health of their members. As with previous contract discussions – where we have successfully fought for our patients – Phoenix Children’s is focused on ensuring payer agreements put kids first and address the specialized nature of pediatric healthcare.
Phoenix Children’s participates with all major health plans except BlueCross BlueShield, so our patients and families have other choices to ensure their access to care. In this open enrollment season, many patient families have options and we encourage them to review a list of in-network plans on our website.”
AZ Blue then released the following statement:
“We’re baffled. Phoenix Children’s Just Turned Down an $80 Million Raise. Phoenix Children’s may be known for great healthcare, but their decisions seem bad for kids who need care and bad for business. As of October 31, 2024, Phoenix Children’s and their providers are officially out of network for some AZ Blue members. Here’s What Happened:
- Last week, Phoenix Children’s turned down a 10% hospital rate increase each year for 3 years, saying no to a $50 million raise.
- In an unexpected move, Phoenix Children’s sent an offer on Tuesday with an increase for some services as high as 30%, resulting in an $80 million raise, plus language changes.
- On Wednesday, in a last-ditch effort to avoid disruption for our members, AZ Blue agreed to Phoenix Children’s financial demands but not their language ultimatum.
- Then, citing contract language, Phoenix Children’s said NO to an $80 million raise over 3 years.*
*And if you’re wondering what their contract language would do, it would remove financial accountability and effectively create cover for inappropriate billing.
AZ Blue teams are standing by to assist members with care coordination, quality provider alternatives, and out-of-state options if that’s what it takes. More at azbluefacts.com/pch.
Frankly their statement is puzzling, and we are still trying to figure out what it means. We are fact checking it now.”
This story was first published on 12News

