Rural health conference makes big impact in its 50 years
Newest Arizona Area Health Education Center is latest example of collaborative meeting leading to solutions for underserved communities.
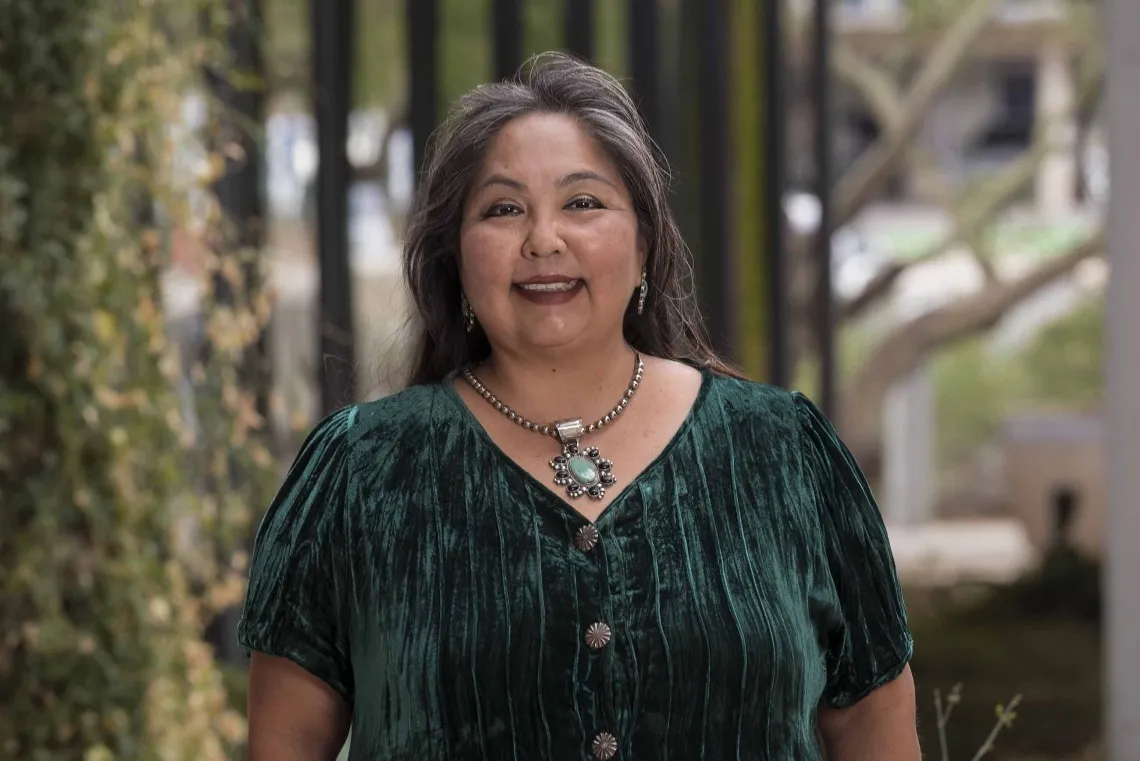
Agnes Attakai, MPA, knows firsthand the health-care hardships that come from living in a remote, impoverished area. She brings that knowledge to her role as a member of the advisory board for American Indian Health Area Health Education Center.
Photo by Noelle Haro-Gomez, UArizona Health Sciences Office of Communications
Agnes Attakai, MPA, grew up in two worlds.
In Southern California, she and her five siblings enjoyed city life. In the summertime, the kids stayed with their grandparents on the Navajo Nation in Arizona, where they had no electricity or running water.
“I grew up going back and forth on Route 66,” said Attakai, who is Navajo and the director of the Circle of Indigenous Empowerment program at the University of Arizona College of Medicine – Tucson’s Sonoran Center for Excellence in Disabilities.
No matter where the kids were, though, one thing remained the same: health care was tricky.
Attakai’s parents didn’t have health insurance, and her grandparents didn’t trust the area Indian Health Service clinic. Attakai can rattle off examples of modern-day failures in the complicated Indian Health Service system. Case in point: Her sister recently thought she was having a stroke, went to the closest Phoenix clinic and ended up being whisked away by ambulance to a specialty hospital. She was stuck with a hefty bill because she went outside her service network rather than her assigned clinic, which was six hours away.
“That is what happens to a lot of people in urban areas because we’re lost,” Attakai said. “We’re not part of the tribal system in our home communities.”
Stories of delayed diagnoses and treatments are common, too, she said. But positive change is in the works for Arizonans, thanks to the American Indian Health Area Health Education Center.
Launched in 2022, the AIH-AHEC is just one of many improvements to come out of the annual Rural Health Conference, a meeting for rural health care providers and service organizations from around the state that’s coordinated by the UArizona Mel and Enid Zuckerman College of Public Health’s Center for Rural Health.
A conference that unites
The 50th annual Arizona Rural Health Conference, held June 4-5 in Flagstaff, Arizona, drew about 475 attendees. The conference, designed to bring together a vast array of groups trying to address unmet needs, is a way to create partnerships to improve the health and health care of those in Arizona’s rural and underserved communities.
“It’s about being part of a larger voice that educates and informs policy for state and even federal deliberations around health policy,” said Dan Derksen, MD, director of the Center for Rural Health and associate vice president for Health Equity, Outreach and Interprofessional Activities at UArizona Health Sciences.
Derksen, is a senior advisor for the UArizona Health Sciences’ Arizona Area Health Education Center Program. He considers the AIH-AHEC, the first of its kind in the state, one of the top accomplishmentsto come out of the Rural Health Conference in its five decades.
“It’s a tangible result that shows the progress being made to address these unmet needs,” Derksen said.
Attakai calls it a “game-changer.”
A long history
Congress created the AHEC program in 1971 to recruit, train and retain a health-care workforce committed to helping underserved populations. The program is designed to use the resources of academic medicine to address local community health needs by creating strong academic-community partnerships.
The new AIH-AHEC is the sixth regional center in Arizona, which is home to 22 federally recognized tribes, and one of only a few in the United States outside of Alaska to focus exclusively on the Native American health care system and its workforce. Native Americans have some of the highest rates of health disparities, poverty and poor health outcomes when compared with other ethnic and minority communities in the U.S., according to the Indian Health Service.
The AIH-AHEC reaches out to young Native students to introduce them to health care careers in the hopes that they’ll become providers who will then serve in their home communities.
“The biggest thing for us is getting Native American youth introduced to health-care careers early and sharing with them the many opportunities that are available,” said Jeff Axtell, MEd, director of the AIH-AHEC at the Arizona Advisory Council on Indian Health Care, which partners with the Arizona AHEC Program to run the regional center.
Another major boost is that the AIH-AHEC will also offer financial support to help defray the costs of schooling, which is another stumbling block for Native American students, Attakai said. She, for example, is the only one of her siblings who pursued higher education.
You can go home
Schooling wasn’t a priority in Attakai’s family. Her parents were part of the Native American boarding school experience, which sent children away from their families to learn vocational skills. Through the federal urban relocation program, which was designed to push Native Americans off reservations and into big cities with the promise of a better life, Attakai’s parents raised their six children in California.
Money was tight. Attakai, who remembers sending cassette tapes back and forth to her grandparents because they didn’t read or write, dropped out of high school to care for her two younger brothers when her parents separated. At 18, she was working in a factory, running a big printing press.
“That was not for me,” said Attakai, who excelled in science and decided to get her high school diploma and go on to college.
At the University of Arizona, Attakai, who is on the AIH-AHEC advisory board, has worked in different roles with tribal communities, from cancer education to training and outreach. She has also recruited Native American students to go into the health profession.
“We have a couple of our Navajo students who are finishing up their residencies. They can’t wait to go home and practice, and that’s great,” Attakai said. “That’s the whole purpose behind these programs. You go away for your education, but you come back home.”

