The uncounted: People of color are dying at much higher rates than what COVID data suggests
The true toll of the COVID-19 pandemic on many communities of color is worse than previously known.

Special to USA TODAY: Published 3:00 AM MST Dec. 28, 2022
It’s not always easy to identify a COVID-19 death.
If someone dies at home, if they have symptoms not typically associated with the disease or if they die when local health systems are overwhelmed, their death certificate might say “heart disease” or “natural causes” when COVID-19 is, in fact, at fault.
New research shows such inaccuracies also are more likely for Americans who are Black, Hispanic, Asian or Native.
The true toll of the COVID-19 pandemic on many communities of color – from Portland, Oregon, to Navajo Nation tribal lands in Arizona, New Mexico and Utah, to sparsely populated rural Texas towns – is worse than previously known.
Incorrect death certificates add to the racial and ethnic health disparities exacerbated by the pandemic, which stem from long-entrenched barriers to medical care, employment, education, housing and other factors. Mortality data from the Centers for Disease Control and Prevention point to COVID-19’s disastrous impacts, in a new analysis by the Documenting COVID-19 Project at Columbia University’s Brown Institute for Media Innovation and MuckRock, in collaboration with Boston University’s School of Global Public Health; the USA TODAY Network; the Arizona Center for Investigative Reporting; Willamette Week in Portland; and the Texas Observer.
The data shows that deaths from causes the CDC and physicians routinely link to COVID – including heart disease, respiratory illnesses, diabetes and hypertension –have soared and remained high for certain racial and ethnic groups.
In Arizona's Navajo and Apache counties, which share territory with Navajo Nation, COVID deaths among Native Americans drove nation-leading excess death rates in 2020 and 2021. While COVID death rates among Natives dropped during the second year of the pandemic thanks to local health efforts, other causes of death such as car accidents and alcohol poisoning increased significantly from 2020 to 2021.
In Portland, deaths from causes indirectly related to the pandemic went up in 2021 even as official COVID deaths remained relatively constant. Black residents were disproportionately impacted by some of these causes, such as heart disease and overdose deaths – despite a county-wide commitment to addressing racism as a public health threat.
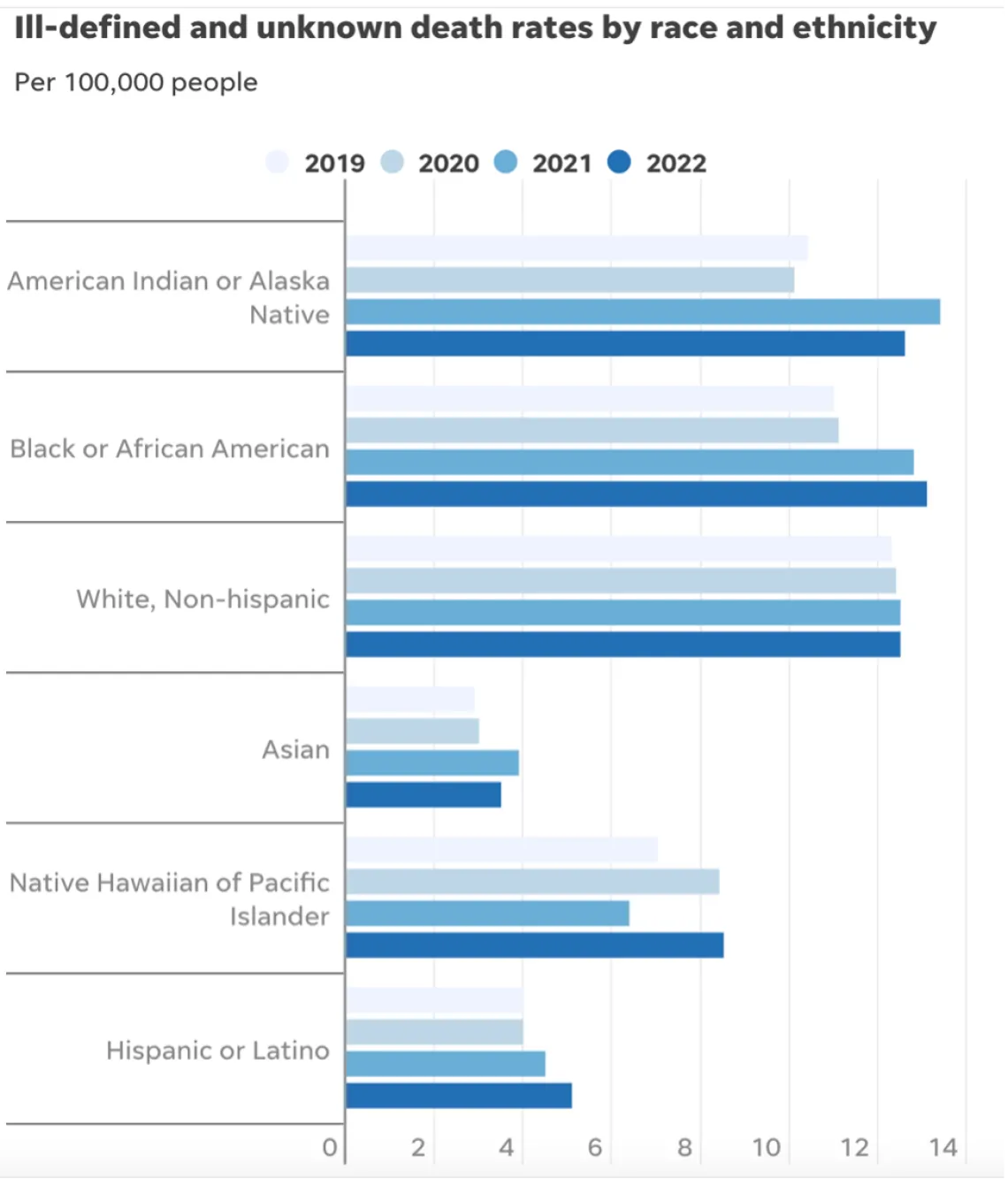
Death rates reflect R-00 to R-99 deaths per 100,000 people, deaths are not age-adjusted. Source: CDC Provisional Mortality Statistics
Source: CDC Provisional Mortality Statistics
UNCOUNTED 2021: Inaccurate death certificates across U.S. hide COVID's true toll
In Texas, smaller, rural counties served by Justices of the Peace were more likely to report potential undercounting of COVID deaths than larger, urban counties served by medical examiners. Justices of the Peace receive limited training in filling out death certificates and often do not have sufficient access to postmortem COVID testing, local experts say.
Experts point to several reasons for increased inaccurate death certificates among non-white Americans. These include resources available for death investigations, the use of general or unknown causes on death certificates, and how the race and ethnicity fields of these certificates are filled out.
Such barriers to accurate death reporting add on to existing health disparities that made non-white Americans more susceptible to COVID in 2021, despite widespread vaccination campaigns and health equity efforts.
“Even if you try to level the playing field, from the jump, certain populations are dealing with things that put them at greater risk,” said Enrique Neblett, a health equity expert at the University of Michigan’s School of Public Health. These issues include higher exposure to COVID, as people of color are overrepresented among essential workers, as well as higher rates of chronic conditions that confer risk for severe disease. “Those things aren’t eliminated just by increasing access to a vaccine,” Neblett said.
It is critical to improve data collection and reporting for deaths beyond those officially labeled as COVID because data is a “major political determinant of health,” said Daniel Dawes, executive director of the Satcher Health Leadership Institute at the Morehouse School of Medicine. Information on how people are dying in a particular community can shape priorities for local public health departments and funding for health initiatives.
“If there is no data, there is no problem,” Dawes said.
Undercounting at the national level
Going beyond the deaths officially attributed to COVID provides a broader picture of the pandemic’s toll on marginalized communities. The U.S. system for investigating how people die is a patchy, uneven network of coroners and medical examiners, which have wildly different resources and training from state to state – or even from county to county.
As a result, researchers often use excess deaths, a measure of deaths that occur above what demographers expect to see in a given time period based on past trends, to examine the pandemic’s overall impact. Nationwide, more than 280,000 excess deaths since 2020 have not been attributed to COVID.
Coroners and medical examiners serving Black communities, in particular, have fewer resources for death investigations, according to an analysis by the Boston University School of Public Health, relying on survey data of death investigations by the Department of Justice. Counties with the highest shares of Black residents had the fewest full-time personnel to investigate each death, the researchers found.
These death investigation offices “may not have the capacity to treat all of these deaths equally,” compared to offices with more staff, said Rafeya Raquib, a research fellow who worked on the analysis.
Also, in the last two years, death investigators have relied more heavily on nonspecific or unknown causes of death for people of color. These causes, called “garbage codes” by researchers, are designed to be used as a last resort when an investigator is unable to determine how someone died.
Garbage codes were a “pretty big problem” before the pandemic, said Laura Dwyer-Lindgren, leader of the U.S. Health Disparities team at the University of Washington’s Institute for Health Metrics and Evaluation. Past analyses going back to the 1990s have found these codes have historically been used more among non-white people.
These inaccurate codes “compromise our ability to say something definitive about a person’s cause of death,” Dwyer-Lindgren said. Garbage code deaths among non-Hispanic white people increased only 1% during the pandemic, compared to the prior two years; among Hispanic, Native, and Asian Americans, they increased by more than 20%.
The Boston University team found this trend was more pronounced among deaths that happened at home, where death investigators with less medical training are in charge.
“Our death investigation system structurally disadvantages communities of color by obscuring the causes of death in those communities, which hinders our policy response,” said Andrew Stokes, a professor in the Department of Global Health at the Boston University School of Public Health and leader of the research team.
Another potential source for undercounting: Race and ethnicity are not always correctly reported on death certificates, especially if the investigator filling out such a certificate is a different race than the person who died. These errors are particularly common for Native Americans, like Mary-Katherine McNatt, a public health expert at A.T. Still University whose research focuses on health disparities.
“Very rarely will someone look at me and say, ‘Oh, she's clearly American Indian,’” she said.
In Native American communities in Arizona, excess deaths remain high
Timian Godfrey, a Navajo assistant clinical professor of nursing at the University of Arizona, traveled to the Navajo Nation in early 2021 to help with its mass vaccination campaign.
The reservation – the largest in the country, with a population over 160,000 and shared territory with Arizona, New Mexico and Utah – was hit hard by COVID in spring 2020. Barriers to health care access and high rates of chronic diseases made the Diné community highly vulnerable; leaders responded with strict lockdowns and other safety measures. Getting vaccines into arms was the next phase of Navajo Nation’s response.
Godfrey said people waited in line for upward of four hours to get their vaccinations. “We heard so many devastating stories, but also the commitment of them knowing that this is what they could do for their family and to protect their loved ones,” she said.
Thanks to these efforts, Arizona’s Native American communities became “pockets of high vaccine areas,” McNatt said. The vaccinations contributed to a sharp decline in COVID deaths and overall excess deaths: In Navajo County, the COVID death rate for Native Americans almost halved between 2020 and 2021, according to analysis of CDC data. In Apache County, the rate dropped by 36%.
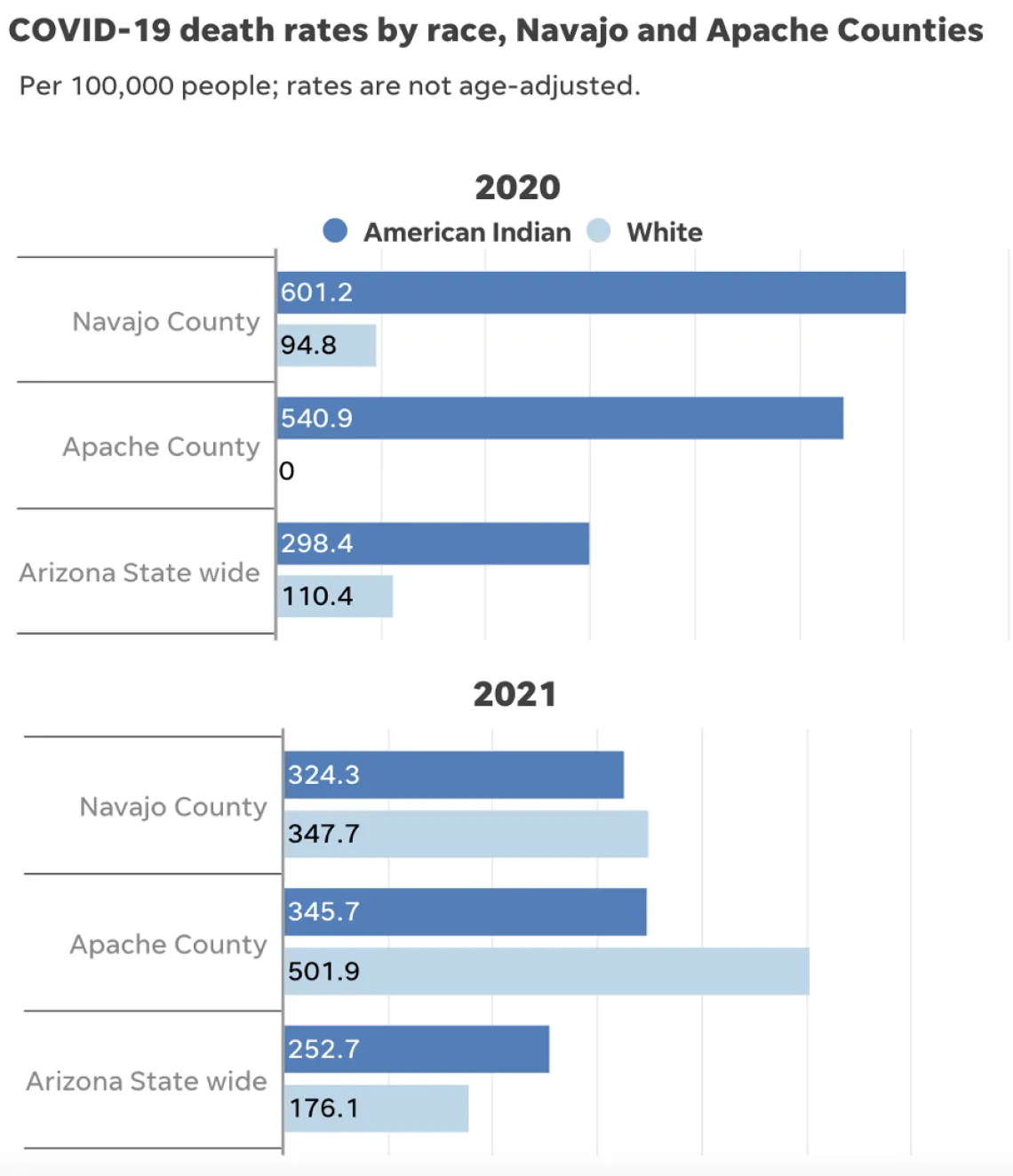
Source: CDC Provisional Mortality Statistics • In Apache County, there were under 10 COVID-19 deaths among white people in 2020, so the CDC does not provide a rate for this year.
But neighboring white communities were more “hostile to masking” and vaccination, said Will Humble, executive director of the Arizona Public Health Association. As a result, white death rates in Navajo County rose by 3.5 times from 2020 to 2021, while white death rates in neighboring Apache County rose by more than five times.
Even as COVID death rates declined for Native Americans, excess deaths in Navajo and Apache counties remained high. In both 2020 and 2021, Apache County had the highest excess death rate of any U.S. county over 30,000 people, while Navajo County had the fourth-highest rate in 2020 and the second-highest rate in 2021.
Arizona counties with high percentages of Native American residents rank extremely high on the CDC’s social vulnerability index, said Dr. Daniel Derksen, director of the University of Arizona Center for Rural Health. “The populations that live in those rural counties tend to be quite vulnerable to things like natural disasters, things like pandemics,” he added, because of numerous factors included in the index calculation, including lack of access to care and populations that skew older.
Despite the vaccination success for this Native American community, legacies of racism and colonialism contributed to continued health problems in 2021, said Emerson, the UNC expert. He pointed to issues such as a lack of clean water and intergenerational households as sources of coronavirus spread in the region. Godfrey said that the high prevalence of chronic diseases in Native Americans, such as diabetes and kidney disease, which are dangerous comorbidities, are also a consequence of colonialism in the country.
» Continue reading at: https://www.usatoday.com/in-depth/news/health/2022/12/28/uncounted-covi…

